- Open-Access Publishing
- Quality and Potential Expertise
- Flexible Online Submission
- Affordable Publication Charges
- Expertise Editorial Board Members
- 3 Week Fast-track Peer Review
- Global Visibility of Published Articles
Lambl's Excrescences and Congenital Heart Disease: Could they Increase the Risk of Ischemic Stroke in Adults? A New Research Perspective
John Jairo Araujo1*, Daniela Alvarez Rendón2, Rafael José Meza3
1Department Pediatric and Adult Congenital Heart Disease, Somer Incare Cardiovascular Center. Rionegro, Colombia
2Department of Clinic Cardiology, Somer Incare Cardiovascular Center. Rionegro, Colombia
3Department of Congenital Heart Surgery, Somer Incare Cardiovascular Center, Rionegro, Colombia
*Corresponding Author: John Jairo Araujo, Department Pediatric and Adult Congenital Heart Disease, Somer Incare Cardiovascular Center. Rionegro, Colombia, E-mail: johnjairoaraujo@gmail.com
Received date: August 02, 2021; Accepted date: August 25, 2021; Published date: September 01, 2021
Citation: Araujo JJ, Rendón DA, Meza RJ. (2021) Lambl's Excrescences and Congenital Heart Disease: Could they Increase the Risk of Ischemic Stroke in Adults? A New Research Perspective. J Card Cardi Sur. 1(2):10.
Copyright: © 2021 Araujo JJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Lambl’s excrescences; Cardiovascular research; Stroke; Congenital heart disease
Abstract
Lambl’s Excrescences (LEx) have a low prevalence in the general population. They occur most frequently in adults over 60 years-old and their importance is related to cryptogenic stroke. Only a few studies have shown the prevalence in the pediatric population, and even more infrequent is to describe them in association with congenital heart disease. This manuscript describes the initial working hypothesis on the little known relationship between LEx and the possible increased risk of ischemic stroke in adults.
Background
Lambl's Excrescences (LEx) are avascular filiform extensions and fibrous projections often containing varying degrees of elastic fibrils. In order of frequency, they affect the mitral valve (68-76%), followed by the aortic valve (38-50%), and, less frequently, the tricuspid valve [1]. Their importance is related to cryptogenic stroke [2].
Introduction
Lambl's Excrescences, also known as strands, occur at valve closure sites, and develop due to the natural wear and tear on the valvular surfaces. They often begin as small thrombi on the endocardial surfaces where the valve edges meet at the valve closure sites (Figure 2). In addition to the heart valves, they can also affect prosthetic valves and endocardial surfaces. Dr. Vilem Dusan Lambl first reported on LEx in 1856 [3]. They are often diagnosed in adults, with increased prevalence after the sixth decade of life, peaking between 61-70 years, and decreasing after the heart valves age and become increasingly calcified, making them hard to see and increasing their under diagnoses. In children, LEx have a very low prevalence (0.9%-2.6%). This supports the age-related "wear and tear" process described in previous studies [4]. They are generally asymptomatic in children and require no intervention. However, in adults, they are associated with thromboembolic events, cerebrovascular accidents, peripheral embolization and acute coronary syndrome [5,6].
Research Hypothesis
Most cases of LEx are diagnosed in adults and in healthy hearts, but they are also associated with rheumatic disease, a history of endocarditis or chronic inflammatory processes [1,7]. We previously published a study of 17 LEx cases which included several pediatric cases related to Congenital Heart Disease (CHD) [8]. Our research group has proposed to answer the question of the congenital origin of LEx, their relationship with CHD and the increased risk of Ischemic Stroke (IS) due to this cause. To date, a bibliographic search has been performed on Google Scholar and PubMed databases in the last 10 years with focus in LEx and CHD (Figure 1 and Table 1).
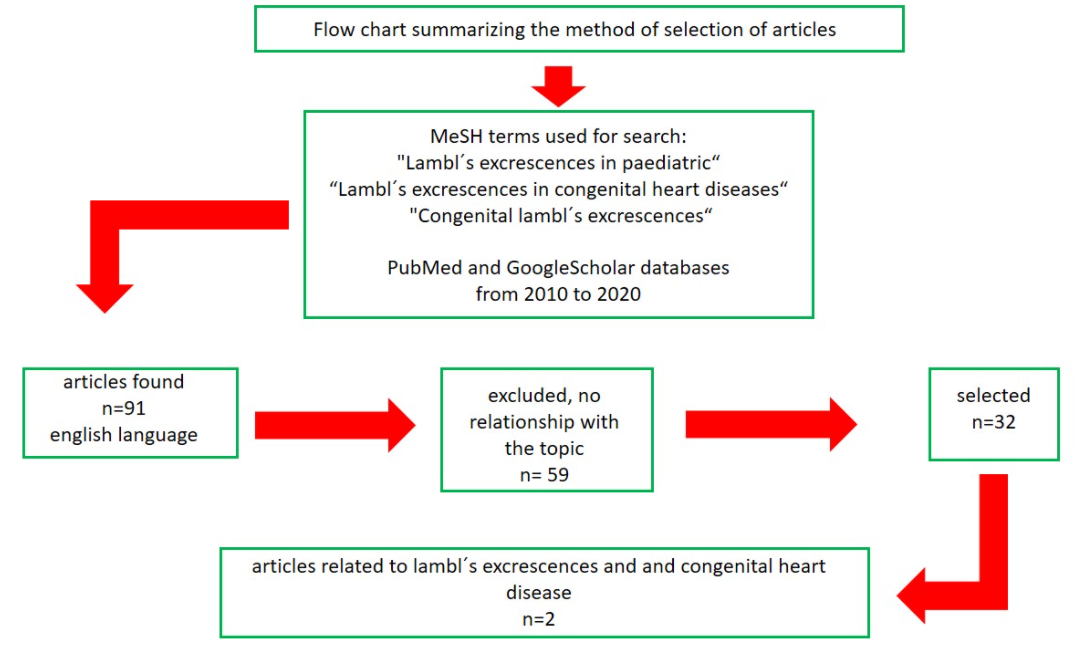
Figure 1: Flow chart summarizing the method of selection of articles.
| Author | Highlights | Follow-up outcome |
| Phillips, et al [4]. |
| Long-term follow-up, there were no clinical events in the 12 children identified with LEx. |
| Araujo, et al [8]. |
| No complications were found throughout the follow-up. |
Research Perspective
One of the reasons our research group became interested in understanding the relationship between LEx and CHD is the scant number of articles published on the topic. As mentioned previously, we have found LEx associated with congenital heart defects, even in newborns. We have therefore wondered if there is a congenital origin of LEx, with this being the main reason. While we still do not have clear evidence of this, we are working on a research project which gathers several LEx cases diagnosed by transthoracic or transesophageal echocardiography during CHD diagnosis or follow up in the pediatric population of our healthcare center. Secondary reason in a future research would be to determine the relationship between LEx and the potential development of IS. Although it is very rare and scarce in children, it becomes more important in the adult population. Therefore, it is important to determine if persistent LEx associated with a repaired or monitored CHD is a cause of IS in adulthood. With the results we might obtain, we could consider the recommendation of whether it is pertinent to carry out an exhaustive search for LEx in all CHD patients, and determine if, once diagnosed in association with CHD, surgical resection is necessary during CHD repair, as we are confirming in several of our cases (Figure 2).
Currently, more than 90% of children with CHD survive to adulthood [9] therefore, the persistence of LEx in adult survivors could explain one of the causes of IS in this population. Recently, Giang, et al. published the most relevant study to date related to IS and CHD. This study compared CHD patients with a control group without CHD. In general, patients with CHD have a five times higher risk of developing IS compared with the population without CHD. A comparison of the two groups (CHD vs. no CHD) showed that the cumulative incidence of IS at age 20 was 0.4% vs. 0.02%; at 50 years was 5.6% vs. 0.4%; and at 75 years was 20.8% vs. 6.8%, respectively [10]. Several known mechanisms and the development of IS are discussed, but the possibility of LEx and CHD is not considered, and this further motivates us to research the topic.
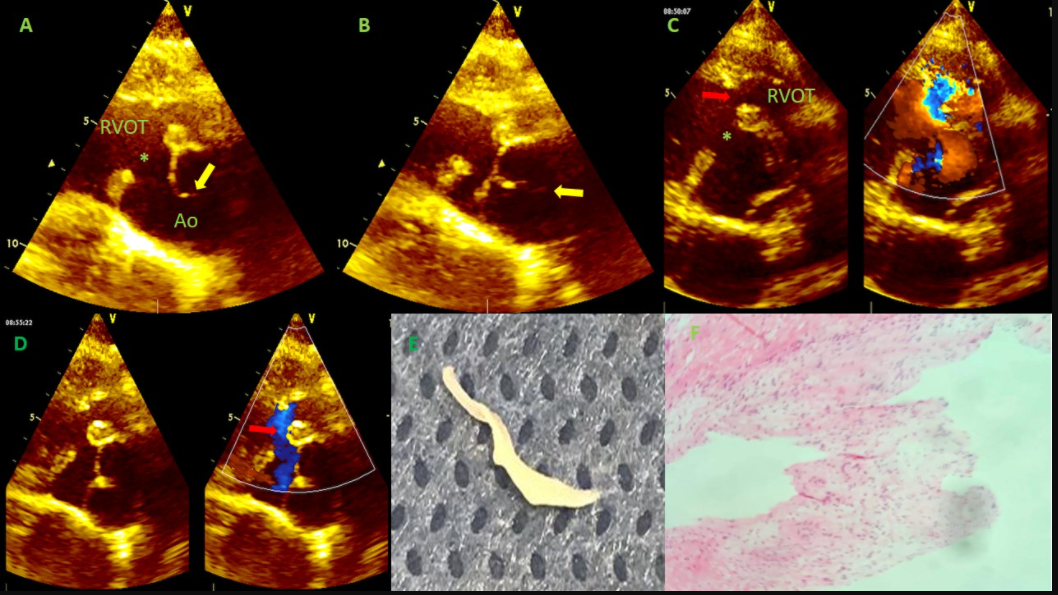
Figure 2: 26-year-old adult with unrepaired tetralogy of fallot, who underwent surgical repair and simultaneous resection of LEx in aortic valve (see below). 2A: Short axis view of the aortic valve in systole (AO). Ventricular septal defect (*) is observed that extends to the Right Ventricular Outflow Tract (RVOT). Yellow arrow shows LEx (fine filaments) that extend over the edge of the right aortic leaflet. 2B: The same in A, dyastole (closed Ao). 2C: Short axis comparative mode color in systole wit focus on RVOT. Red arrow shows the hyperrophic infundibular septum, displaced anterior and right in RVOT. At this point there is an obstruction. 2D: The same view in D, the red arrow shows blood in diastole causing shear stress on the aortic valve, which is a described cause of the wear process and the development of Lex. 2E: Gross anatomic specimen of the LEx removed during surgical repair of CHD. 2F: microscopic examination of the tissue with hematoxylin eosin staining revealed that the structure consisted of focally hyalinized dense connective tissue with little inflammatory infiltrate.
Conclusion
Lambl's excrescences have a low prevalence in the pediatric population and are frequently benign; thus, their detection is not routinely included in echocardiographic studies. However, in previous cases, we have noted the presence of LEx associated with repaired or unrepaired CHD, which suggests that the prevalence of LEx may be greater. At the same time, if CHDs are the most common congenital malformation and LEx may be associated with these congenital defects, we could conclude that it is necessary to surgically resect LEx during CHD repair. This is based on the fact that, today, more than 90% of children with CHD survive into adulthood, and IS is a common problem in adults. Our ongoing study seeks to explain the relationship between LEx and CHD, determining if they are coincidental or if they are a part of the CHD itself (congenital origin). We hope to conclude this study and contribute the answers to the questions proposed in the working hypothesis. This could provide guidelines for the surgical management of CHD and more explanations of IS in adults.
Acknowledgments
We thank to Nadir Mari L and Cito Pat Laboratory for pathologic study in this case.
Conflict of Interest
The authors have no conflict of interests related to this publication.
Funding
There was no private or public sector funding for this research.
Authors’ Contribution
- John Jairo Araujo: Performed echocardiogram, wrote the paper
- Daniela Alvarez Rendón: Wrote the paper
- Rafael Jose Meza: Performed surgery and observer
References
01. Ammannaya GKK. Lambl's Excrescences: Current Diagnosis and Management. Cardiol Res. 10(4): 207-10 (2019).
02. Kalavakunta JK, Peddi P, Bantu V, Tokala H, Kodenchery M. Lambl's excrescences: A rare cause of stroke. J Heart Valve Dis. 19(5): 669-70 (2010).
03. Lambl VD. Papillare exkreszenzen an der semilunar-klappe der aorta. Wien Med Wochenschr. 6: 244-247 (1856).
04. Phillips AL, Qureshi MY, Eidem BW, Cetta F. Lambl’s excrescences in children: Improved detection via transthoracic echocardiography. Congenit Heart Dis. 13(2): 251-53 (2018).
05. Kariyanna P, Jayaranagaiah A, Kats Y, Sharma A. Recurrent cardio-embolic cerebrovascular accidents due to Lambl’s excrescences? Am J Med Case Rep. 4(3): 93-6 (2016).
06. Kariyanna P, Jayarangaiah A, Rednam C, Hegde S, Marmur JD, et al. Lambl's excrescences and stroke: A scoping study. Int J Clin Res Trials. 3(2): 127 (2018).
07. Roldan C, Schevchuck O, Tolstrup K, Roldan P, Macias L, et al. Lambl’s excrescences: Association with cerebrovascular disease and pathogenesis. Cerebrovasc Dis. 40(1-2): 18-27 (2015).
08. Araujo JJ, Rahimy T. Lambl’s excrescences in congenital heart disease and other clinical situations: A Series of 17 Cases. ERHM. 3(4): 1-5 (2018).
09. Araujo JJ. Adults with congenital heart disease in the Americas-where we are today and where we are heading: A general view of the inter-American Adult Congenital Heart Disease Council. 3(3): 4-5 (2020).
10. Giang KW, Fedchenko M, Dellborg M, Eriksson P, Mandalenakis Z. Burden of ischemic stroke in patients with congenital heart disease: A nationwide, case-control study. J Am Heart Assoc. 10(13): e020939 (2021).